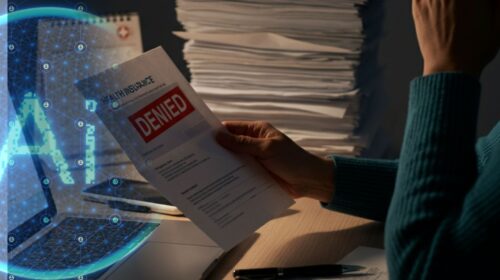
Artificial intelligence (AI) has revolutionized many industries, but its use in health insurance claims processing is stirring sharp debate. Health insurance giants like Cigna, Humana, and UnitedHealth Group are facing serious allegations over their use of algorithm-driven systems to deny claims at a staggering rate. With lives at stake and lawsuits piling up, the practice has raised deep ethical and legal concerns. The Allegations Against Industry Leaders The controversy largely centers on accusations that AI algorithms are being used to wrongfully deny claims, often in mere seconds. One lawsuit claims…
Read MoreTag: patient impact
Why New Insurance Rules Could Make Weight Loss Treatments Harder to Access
Independence Blue Cross Restricts Weight Loss Drug Coverage Starting January 1, 2025, Independence Blue Cross (IBX), the largest health insurer in southeastern Pennsylvania, will no longer cover certain weight loss medications, including GLP-1 receptor agonists like Wegovy and Ozempic, when prescribed solely for managing weight. The company will continue covering these medications for individuals with FDA-approved conditions such as Type 2 diabetes or cardiovascular disease. This change impacts both group and individual commercial plan holders, shifting the full cost of these drugs—ranging from $700 to $1,350 per month—to patients who…
Read More